Non-Surgical Management of Legs Varicose Veins and Swelling
Varicose veins are one of the most common health problems. It is also a significant aesthetic issue. It is estimated that almost close to one-fourth of adults in the US have varicose veins. If less significant issues like telangiectasis and reticular veins are counted, then the condition is present in almost 80% of adults. It is also more common among women.
Fortunately, only a small number of people develop severe signs and symptoms of venous insufficiency. Nevertheless, a considerable number of people (about 2 million) develop symptoms like discomfort, burning sensations, pruritis, irritated skin, and even ulcers.
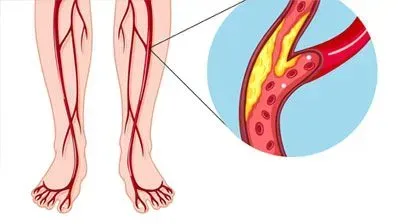
Varicose veins most commonly affect the legs. It is because blood has to flow against the gravity in the leg’s veins, causing considerable stress. Moreover, leg veins are unique in many other ways. For example, they have valves to prevent the backflow of the blood. In varicose veins, these valves are severely affected, resulting in blood accumulation, causing heaviness, fatigue, cramping, changes in the skin, and leg ulcers.
What causes varicose veins?
The cause of varicose veins is a subject of considerable debate. However, it appears that genetic weaknesses contribute considerably to the condition. Due to genetic reasons, some people have weaker venous valves, vascular walls, and higher venous pressure.
The condition is often made worst by certain lifestyle and environmental factors. Thus, it worsens with age, increased abdominal pressure due to obesity, pregnancy prolonged standing, pregnancy, to name a few.
Non-surgical options for the treatment of varicose veins
If venous veins are treated in a timely manner, they rarely need surgical correction these days. Instead, varicose veins can be corrected using minimally invasive methods. Most people would perhaps start with some conservative methods like bandages. However, ultimately, varicose veins would progress in requiring specialized treatment in clinics – called interventional or minimally invasive methods.
Conservative methods
It is highly recommended to start with lifestyle modifications like quitting smoking, avoiding prolonged standing. One may also need to avoid exercises that put unusual strain on the legs.
Elevation of legs may help relieve symptoms. It may be especially useful for pregnancy-associated varicose veins.
Similarly, compression therapy may help relieve symptoms. However, it is worth understanding that it is only a temporary measure. There is no evidence that the use of compression stockings helps in the long run.
Many people would like to use medications. However, it is worth knowing that no pharmacological drug can reverse the condition. In fact, no medicine can effectively prevent the progress of the disease for long enough. Nevertheless, some natural remedies may help symptomatically, like Diosmiplex (Vasculera), a prescription formulation of natural origins (not a chemical drug).
Certain supplements, called phlebotonics, may help relieve symptoms temporarily. In addition, they may have some role in the management. Thus, one may use flavonoids like rutin, diosmin, grape seed extract. Similarly, there is some evidence in favor of horse chestnut seed extracts.
These natural remedies may work for many, providing relief. However, in some, the condition would progress, and symptoms worsen. In such cases, it is better to get treated with the help of minimally invasive methods.
Interventional or minimally invasive methods
These days use of surgical methods for managing varicose veins is rarely required. Most varicose veins can be effectively treated using interventional or minimally invasive procedures. These methods use special equipment for the treatment. They are still invasive, but they involve only making a small cut, unlike surgery. Thus, the procedure is minimally traumatic.
Interventional treatment can be broadly divided into thermal ablation and endovenous Sclerotherapy.
Thermal ablation, as the name suggests, involves using the heat created by high-energy radio waves or lasers. In some cases, doctors may even use lasers externally, like in superficial spider telangiectasias. However, in most cases, they would use an endovenous catheter.
Endovenous catheter involves making a small cut and then introducing either laser or radio waves producing equipment into the veins. In addition, doctors would often use ultrasound to visualize how the catheter is moving in the veins.
Once the catheter reaches the place, they use either laser or radio waves to generate heat. This, almost immediately, coagulates the blood and closes the vein. Once the vein is closed, the body can use other healthy veins for blood flow.
Since it requires only a tiny cut, local anesthesia is just enough. It means that the procedure does not last long. A person can start walking after the procedure and return home on the same day.
Endovenous sclerotherapy may be needed in some cases. Though thermal ablation is more commonly used, endovenous sclerotherapy works better in some cases. For example, it is generally preferred for small to medium-sized varicose vein issues or to treat recurrent varicose after surgery.
Quite like thermal ablation, this method also involves making a minute cut under the local anesthetics and then introducing the catheter. Again, the procedure is quite similar to thermal ablation. However, instead of lasers or radio waves, doctors use a so-called sclerosing agent. It is a kind of foam that is used to block the arteries. Thus, this foam works like a sealing agent.
People would frequently like to know which method is better than another. It is vital to know that studies do not show that any method is superior to another. The choice of methods is made by a doctor. Specialists can only tell which method will work better for a specific patient.
These interventional or minimally invasive methods have almost completely replaced surgery these days. A systemic review of numerous clinical studies suggests that interventional procedures are as good as surgery for the larger varices, like saphenous vein varices. However, they have much faster recovery times.
References
- Piazza G. Varicose Veins. Circulation. 2014;130(7):582-587. doi:10.1161/CIRCULATIONAHA.113.008331
- Jaqueline Raetz MD, Wilson M, Collins K. Varicose Veins: Diagnosis and Treatment. AFP. 2019;99(11):682-688.