Leg Ulcers Due to Poor Circulation in Michigan
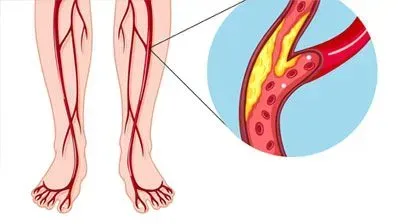
Leg ulcers are one of the most prominent signs of peripheral vascular disease (PVD). However, it is worth understanding that poor blood flow circulation may occur both due to peripheral arterial disease (PAD) or peripheral venous disease (PVD).
These conditions affect very different kinds of blood vessels. Nonetheless, they might share many traits. After all, changes in both the arterial and venous flow would cause disruption in the blood flow and thus leg ulcers.
Nonetheless, these conditions are significantly different from each other. In the case of PAD, blood is not reaching the legs in sufficient volume. It means pain in the calves when walking and heaviness in the leg. Such pain gets worse on physical exertion.
However, in the case of blockage of veins, blood flow to the legs is still more or less adequate, but it fails to return to circulation. This causes an accumulation of fluids and other materials in the lower extremities, causing edema. When obstruction of arteries or veins becomes too severe, a person may develop leg ulcers.
Both PAD and PVD may cause non healing leg and foot ulcers, but symptoms may differ
Although both PAD and PVD may cause leg ulcers, they have different symptoms.
In the case of PAD, there is just not enough blood flow to the lower legs. It means pain in the leg when active but relative relief on rest. This also makes the legs feel weak and numb, and there are changes in skin color, temperature, weak pulse, and formation of dead tissues.
Arterial ulcers also differ a bit with red or yellow sores, hair-less skin, deep wounds and yet lack of bleeding, and legs are cold on touch. These ulcers are also more likely to form on the outer side of the feet, ankle, heels, or toes.
In the case of PVD, symptoms are slightly different. There are visual changes like veins appearing on legs, spider veins, and even varicose veins. Apart from that, there is swelling of the legs, and they feel heavy. In addition, a person is prone to leg cramps. Unlike PAD, pain may worsen by sitting for long in the same position.
Venous ulcers also differ from arterial ulcers. They are less likely to be painful. Nonetheless, there is significant inflammation, swelling, hardening of the skin, and discharge from the ulcers.
What causes peripheral vascular disease?
Although local symptoms like leg ulcers may sound alarming, it is vital to understand that peripheral vascular disease is secondary to systemic disorders. For both arterial and venous diseases, genetic causes are a predisposing factor. However, arterial, and venous diseases occur due to different reasons.
When it comes to arterial disease, the condition mainly occurs due to atherosclerosis. Thus, risk factors are conditions like diabetes, smoking, high blood pressure, trauma, and vasculitis, to name a few.
In the cases of the veinous disease, causes could be varicose veins, trauma, obesity, blood clotting disorders, deep vein thrombosis, heart failure, and other issues.
Diagnosis of peripheral vascular disease
Diagnosing the peripheral vascular disease would need both diagnosing the systemic disorder and local inspection and imaging. Once the chronic leg ulcer is diagnosed and confirmed to be due to vascular deficiency, doctors would try to determine if it is due to a venous or arterial condition.
Generally, diagnosing the ulcer related to PVD is more straightforward, and extremities inspection can suggest venous disease. Nonetheless, some conditions like deep vein thrombosis would require more thorough testing. For example, blood tests may help diagnose clotting defects.
In the case of arterial disease, the diagnostic approach is more complex. For example, there might be pain on palpation, muscle atrophy, cold skin, absence of pluses, and more on physical examination.
Although signs and symptoms may help, generally, doctors would opt for imaging methods like doppler ultrasound imaging, venography, and VQ scan (a test used to detect a blood clot in the lungs).
Treatment approach to leg ulcers due to poor circulation
Although vascular management is the mainstay of the treatment of leg ulcers due to poor circulation, many other treatments are needed. Thus, multi-specialist teams manage chronic leg ulcers. This would involve treatment for various chronic ailments, the use of antibiotics, physical treatment, and more.
It is vital to understand that taking care of leg ulcer wounds is quite challenging. Moreover, therapy for ulcers due to venous causes and arterial causes may differ considerably.
Thus, doctors may use anti-coagulation therapy, sclerotherapy, radiofrequency ablation, endovenous laser treatment, and so on in the case of venous ulcers. Most often, the aim of treatment is mainly to improve blood flow and close the defective veins.
When it comes to arterial disease, the approach differs as the prime aim is to open the closed artery or bypass it so that blood flow can be revived. Thus, doctors may use balloon angioplasty, stenting, and even bypass surgery. The choice of treatment would depend on the severity of the condition.
However, that is not all, and doctors may need to carry out other surgical interventions to promote healing, like wound debridement (removing dead tissues and promoting healing). Some people may also require plastic surgery and other similar interventions.
To conclude, leg ulcers may occur due to many disease conditions like diabetes, varicose veins, deep vein thrombosis, atherosclerosis, etc. In addition, these non healing leg and foot ulcers may occur due to either arterial or venous insufficiency caused by these illnesses. Thus, the treatment must focus on managing the systemic ailment that caused the vascular disease and endovascular intervention to promote quick healing of leg ulcers. Endovascular interventions can also help prevent future episodes and provide prolonged relief.
References
- Zemaitis MR, Boll JM, Dreyer MA. Peripheral Arterial Disease. In: StatPearls. StatPearls Publishing; 2022. Accessed April 11, 2022. http://www.ncbi.nlm.nih.gov/books/NBK430745/
- Meissner MH, Moneta G, Burnand K, et al. The hemodynamics and diagnosis of venous disease. Journal of Vascular Surgery. 2007;46(6, Supplement):S4-S24. doi:10.1016/j.jvs.2007.09.043
Why Choose Advanced Veins and Vascular Management for Leg Ulcer Treatments?
Leg ulcers are painful sores on the legs, often due to poor circulation. If left untreated, they can become chronic, causing discomfort, infection, and complications. Most non healing leg and foot ulcers stem from venous insufficiency, arterial problems, or diabetes. Understanding the causes and receiving proper treatment is vital to prevent them from worsening.
At Advanced Vein and Vascular Management, our professionals are experts in diagnosing and treating leg ulcers. We understand that each case is unique and requires an individualized approach for effective healing. Venous ulcers, caused by malfunctioning valves in the veins, are a common form of leg ulcers. Blood pools in the lower limbs, leading to pressure and the breakdown of the skin, resulting in ulcers. We offer a range of treatments that target the root cause of the ulcer, not just the symptoms.
One standard treatment method is compression therapy, which helps improve blood flow by applying pressure to the leg, reducing swelling, and promoting healing. In more severe cases, minimally invasive procedures, such as endovenous laser treatment (EVLT) or sclerotherapy, may be necessary to correct venous insufficiency. These advanced treatments close off faulty veins, allowing blood to reroute through healthier pathways and reducing the risk of future ulcers.
What truly sets Advanced Vein and Vascular Management apart is our commitment to comprehensive and ongoing care. Non healing leg and foot ulcers often require long-term management to prevent recurrence. Our team works closely with patients, providing personalized care plans that include lifestyle recommendations, wound care, and regular follow-ups. This comprehensive approach ensures that healing is sustained and the risk of new ulcers is minimized.
By addressing the underlying vascular issues and providing proper wound care, Advanced Vein and Vascular Management can help patients regain comfort and prevent further complications. If you have a leg ulcer, consult these professionals to start your journey toward effective treatment and recovery.
Leg Ulcers FAQ
How can regular exercise benefit those with leg ulcers?
Regular low-impact exercises like walking, swimming, or cycling may help improve blood circulation, which can be beneficial for managing leg ulcers. Better circulation can reduce swelling and support the healing process. Additionally, compression stockings during exercise may enhance circulation and provide additional support. It’s advisable to consult a vein disease doctor for personalized exercise and compression therapy recommendations as part of a nonhealing leg ulcer treatment plan.
What role does diet play in managing leg ulcers?
A diet rich in vitamins, especially Vitamin C and Zinc, may support the healing of leg ulcers. Vitamin C aids tissue repair, while Zinc is essential for skin health. Maintaining a healthy weight through balanced nutrition can reduce pressure on the legs, potentially improving ulcer outcomes. Staying hydrated is also essential for circulation and overall healing. For personalized dietary advice, consider consulting a vein disease doctor to integrate these elements into your treatment plan.
How does smoking affect leg ulcers and overall health?
Smoking can impair circulation by narrowing blood vessels, which may delay the healing of leg ulcers. Improved circulation is essential for effective treatment, and quitting smoking can help enhance blood flow and support healing. Additionally, quitting smoking offers broader health benefits, such as better heart and lung function. For comprehensive support and advice on managing leg ulcers and quitting smoking, consult with a vein disease doctor and explore treatment options at Advanced Vein and Vascular Management.